
by Dr. Delvadia, DPM | May 15, 2021 |
Why elderly foot care should be a priority? You may think a great deal about your overall health and how to stayhealthy, but you might forget about your feet. The truth is, if your feetaren’t healthy, you can find yourself immobile and housebound or even worse....

by Dr. Delvadia, DPM | Apr 26, 2021 |
What is a Clinical Pedicure? A Clinical Pedicure is a perfect way to relax and treat your feet to the care and attention they need. It can complement medical treatments of foot ailments by preventing foot disorders and can be helpful in supporting healing. ...
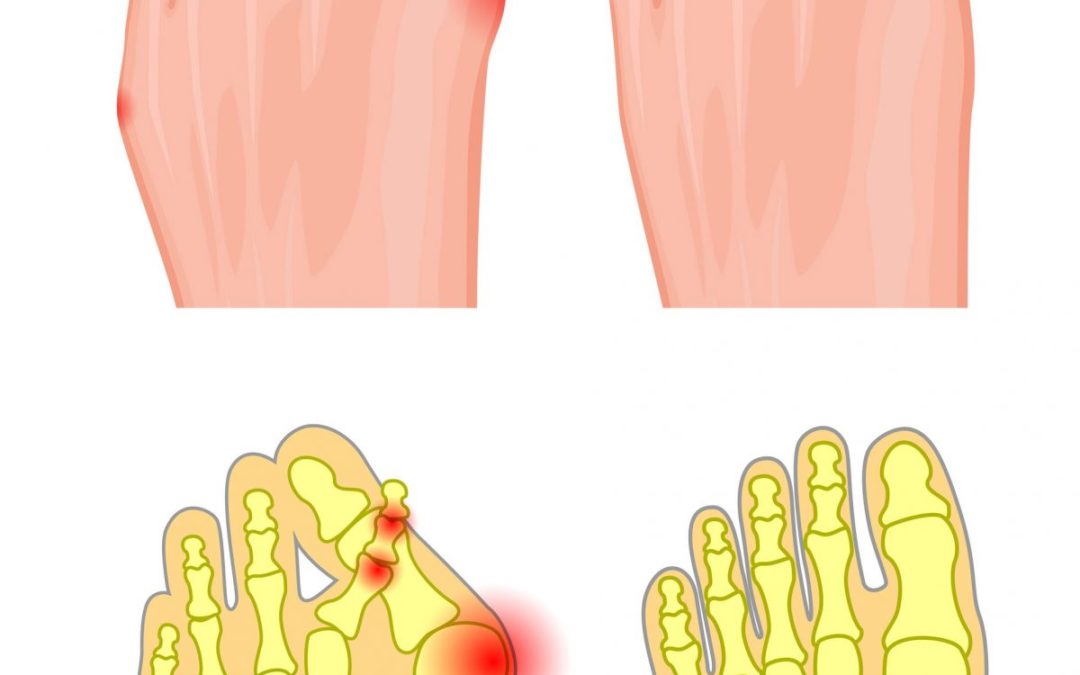
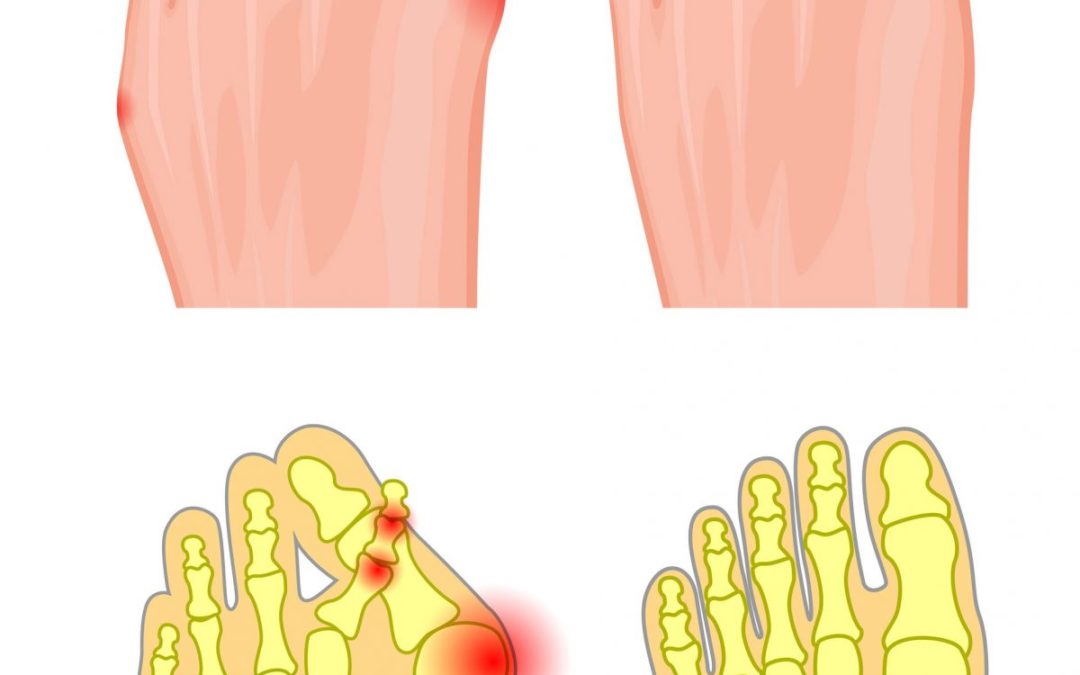
by Dr. Delvadia, DPM | Mar 22, 2021 |
What Is A Hammer Toe? A hammertoe, or claw toe, describes a condition where the toe(s) become buckled, contracted, or crooked. The toe could even cross over an adjacent toe, which is called a cross over toe. Any of the toes may be affected, but the second and Fifth...

by Dr. Delvadia, DPM | Aug 27, 2020 |
What is a Medicated Pedicure? A Medicated Pedicure is the perfect way to relax and treat your feet to much-needed care and attention. It can complement medical treatments of foot ailments by preventing foot disorders and can be a helpful support in healing. It’s...

by Dr. Delvadia, DPM | Aug 27, 2020 |
What is a Deep Pedicure? A Deep Pedicure is the perfect way to relax and treat your feet to much-needed care and attention. It can complement medical treatments of foot ailments by preventing foot disorders and can be a helpful support in healing. It’s the...

by Dr. Delvadia, DPM | Aug 27, 2020 |
Can You Get Fungus From Nail Polish? Toenail fungus infections are a common foot health problem and may continue for years without ever causing pain. The disease, characterized by a change in a toenail’s color, is often considered nothing more than a flaw or...






![podiatryGroup-Logo[1] Logo](https://www.podiatrygroupofgeorgia.com/wp-content/uploads/2020/07/podiatryGroup-Logo1.png)